The advantages of an implant with a zirconia collar – Dr Massimo Palermo
Featured Products Promotional FeaturesPosted by: Dental Design 26th September 2019


Dr Massimo Palermo explains through a case study how a tissue-level implant with a zirconia collar can help clinicians regenerate and preserve bone, while also encourage effective healing of the gingiva for superior soft tissue management.
In May 2013, a 46-year-old female patient presented with an infection (Figure 1) near the apex of the LR6 tooth root. A treatment plan was formulated and discussed with the patient, which involved extraction of the LR6 and placement of a 4mm diameter by 10.5mm length TBR Z1 dental implant.

Figure 1: Infected tooth
A radiograph (Figure 2) was taken which showed that the patient had insufficient bone quality and quantity, as the top of the cortical bone was not level. In order to preserve the socket, extraction of the LR6 was performed and a collagen sponge made of lyophilized non-denatured type-I collagen extracted fromequine Achilles’ tendon (Condress) was placed, in order to encourage accelerated healing[i]of the supporting bone so that an implant could be placed.

Figure 2: Radiograph of the infected LR6
Implant placement
Five months following extraction, a radiograph (Figure 3) taken in preparation for implant placement demonstrated imperfect bone levels, despite the socket preservation procedure. The decision was therefore made to perform guided bone regeneration (GBR) at the time of implant placement.

Figure 3: Post-extraction and socket preservation
The implant surgery involved making an incision in the gingiva to raise a full thickness flap, which provided access to the bone. A hole was drilled in the surgical site before the implant was placed at the pre-determined depth and diameter. At this time, a synthetic bone graft made from B-TCP (Graftek) was carried out and a type-I equine collagen membrane was placed to prevent the grafted site being colonized by soft tissue.[ii]A periosteal-release incision was created to obtain a tension-free closure over the cover screw of the implant.[iii],[iv]
Having later achieved excellent bone and soft tissue regeneration, a second surgical step was required. A circular opening was created with a diode laser so that the healing abutment (Figure 4) could be placed. While this second surgical step is not normally indicated when using the Z1 implant – the gingiva usually grows around the transgingival zirconia collar naturally[v]– it was selected in this case in order to preserve the maximum amount of soft and hard tissue.

Figure 4: Healing abutment placed
Restoration
Six months post-implant surgery, a radiograph (Figure 5) demonstrated excellent bone growth that fully supported the implant. Figure 6 shows that the implant had healed well with no sign of infection or gingival inflammation. The Z1 implant facilitated enhanced healing of the gingiva, particularly around the zirconia collar.

Figure 5: Radiograph of implant placed

Figure 6: Six months following placement of implant
In fact, healing had been so successful that the gingiva had begun to grow over the healing cap, so a laser was used to cut back the soft tissue to improve access to the implant component. Unlike traditional bone-level implant solutions that often require two-stage surgery in order to place the restoration (as a result of the gingiva healing over the implant), the Z1 implant usually only requires one-stage surgery. This makes it more comfortable for the patient and more time-efficient for the practitioner. However, this case was an exception because the full thickness flap and the GBR procedure carried out during implant placement – combined with the outstanding soft tissue integration properties of the zirconia collar – led to excessive gingival proliferation which required laser gum surgery.
The healing cap was then removed and figure 7 shows that the white collar of the implant could be seen. If a traditional titanium implant solution is used, the greyish hue of the metal component can become visible in the case of thin gum or gingival recession. The A2 shade of the Z1 implant’s collar ensures natural transparency.

Figure 7: Healing abutment removed
Implant restoration
After two weeks, the soft tissue had healed from the laser treatment and several months after implant placement, the gingiva remained pink and healthy.
The healing cap was removed in order to fit a TBR Swiss clip direct impression coping (Figure 8). This does not involve the use of a screw and is a simple, quick impression-taking solution that combines the benefits of both direct and indirect techniques. In particular, it is ideal for closed-tray methods involving single-unit implants, meaning clinicians do not have to rely on a customised tray. An impression (Figure 9) was then taken, which was sent to the laboratory technician to create a model (Figures 10 and 11). The technician fabricated a zirconia crown (Figures 12 and 13), which was sent back to the practice for a try-in with the patient to ensure a satisfactory fit (Figures 14, 15, 16, 17 and 18).

Figure 8: TBR Swiss clip impression coping

Figure 9: Impression material with impression coping
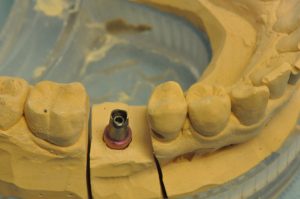
Figure 10: Abutment on impression model

Figure 11: Overview of abutment on impression model

Figure 12: Zirconia crown on impression model

Figure 13: Overview of zirconia crown on impression model

Figure 14: Implant prior to fitting the crown

Figure 15: Abutment placed

Figure 16: Overview of abutment placed

Figure 17: Crown fitted to the abutment

Figure 18: Overview of the final restoration

Figure 19: Comparison of the crown to the adjacent natural teeth
Once this was confirmed, temporary cement (ImplaCem Automix Precision) was used to secure the prosthesis to the abutment. Although this material is very strong and demonstrates long-term stability comparable to permanent cement, it enables easy removal of the crown if necessary.
Traditional abutments are usually the same diameter as the implant component. With regard to the Z1 implant, the abutment is always smaller than the zirconia collar, so that masticatory forces can be absorbed by the abutment and the titanium core of the implant. In the case of a bone-level implant, there would be a smaller margin for the crown to rest on, corresponding to the shoulder of the abutment. However, the tissue-level Z1 implant – whose zirconia collar ensures an optimal cervical adaptation of the crown and, in our case, a ceramo-ceramic continuity between the implant collar and the crown – helps prevent any gingival infiltration. In addition, conventional implant abutments usually cover the implant components completely, while the Z1 collar pushes the gingiva laterally, acting like a gingival scaffold that further promotes optimal gingival health.
Result
Following completion of treatment, the zirconia collar implant provided results comparable to a natural tooth. As figure 19 demonstrates, the emergence profile of the implant was very good and looked like the adjacent natural gingiva. Two radiographs were taken – one in 2018 (Figure 20) and the other in 2019 (Figure 21). Both of these showed the same result five and six years respectively following implant placement. In fact, the peak of the bone near the collar is in the same condition as when the implant was first placed. There is excellent gingival integration (Figure 22), with no bone resorption near the zirconia collar. An increase in keratinised gingiva can be seen just below the coronal margin at the level of the implant’s zirconia collar. Evidently, the patient had very good oral hygiene to help maintain a healthy implant, but this is not the only reason for lack of bone resorption and gingival recession. The design of the Z1 implant helped to ensure there was no infiltration of bacterial pathogens, thereby reducing the risk of inflammation and peri-implantitis, which is one of the main causes of implant failure.[vi]The Z1 implant not only enables clinicians to achieve effective osseointegration, but also periointegration.
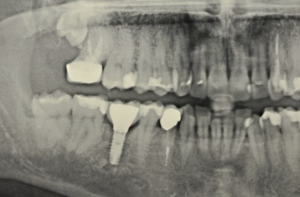
Figure 20: Panoramic radiograph of the implant and crown

Figure 21: Radiograph taken 6 years post-implant placement

Figure 22: The result 6 years post-implant placement
Conclusion
In the case of a titanium bone-level implant, there is often slight bone resorption and, therefore, soft tissue recession.[vii],[viii]This was not an issue in regards to the TBR Z1 implant, which performed beyond initial expectations. As a ‘soft-tissue friendly’ solution, it encourages gingival growth for effective maintenance over time[ix], as was evident in the case. It took a whole year to complete treatment because it was difficult for the patient to attend appointments at the preferred time. However, the process concluded in June 2014 and the patient is still very happy with the final result, which remains highly aesthetic and functional.
For more information on the Z1 implant, visit tbr.dental, email support@denkauk.comor call 0800 707 6212
Author bio:
Dr Massimo Palermo, MDDS, has been working alongside TBR for over 25 years. He specialised in periodontal regeneration and reconstructive plastic surgery at Florence University. He practises from a private clinic in Rome, focusing on oral rehabilitation surgery, guided bone regeneration (GBR), guided tissue regeneration (GTR), and dental implantology. At the Sapienza University of Rome, he collaborates on research projects with the Department of Dentistry and Maxillofacial Sciences. He also works with the Faculty of Economics and Commerce, as well as the Faculty of Medicine and Surgery, contributing to research on bioethics and management in health economics.
Beyond this, Dr Palermo participates in both national and international dental courses. He trains other dentists in implant surgery, as well as GBR and GTR techniques, having authored and co-authored numerous articles on the same topics. Dr Palermo also lectures on a wide range of subjects, including oral surgery, periodontal surgery, implant surgery, regenerative bone surgery, unconventional medicine, bioethics, dental marketing and management.
References
[i]Beghé, F., Menicagli, C., Neggiani, P., Zampieri, A., Trallori, L., Teta, E., Rosini, S. Lyophilized non-denatured type-I collagen (Condress) extracted from bovine Achilles’ tendon and suitable for clinical use. Int J Tissue React. 1992;14 Suppl:11-9. [Last accessed: 20.12.18]
[ii]Elgali I, Omar O, Dahlin C, Thomsen P. Guided bone regeneration: materials and biological mechanisms revisited. Eur J Oral Sci. 2017;125(5):315-337. [Last accessed: 20.10.18].
[iii]Romanos GE. Periosteal releasing incision for successful coverage of augmented sites. A technical note. J Oral Implantol. 2010;36(1):25-30. doi: 10.1563/AAID-JOI-D-09-00068. [Last accessed: 20.12.18]
[iv]Steigmann M, Salama M, Lau K. (2012) Periosteal pocket flap for horizontal bone regeneration: A case series. Int J Perio Res Dent. 32(3):311-20 https://www.researchgate.net/publication/221694653_Periosteal_Pocket_Flap_for_Horizontal_Bone_Regeneration_A_Case_Series[Last accessed: 20.12.18]
[v]Bianchi, A. E., Bosetti, M., Doci, G., Sberna, M. T., Sanfilippo, F. and Cannas, M. (2004) The Zirconia solution: increasing osteoblasts and fibroblasts adhesion and proliferation
[vi]Prathapachandran, J. and Suresh, N. (2012) Management of peri-implantitis. Dental Research Journal. 9(5): 516-521. Link: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3612185/. [Last accessed: 01.10.18].
[vii]Vouros, I. D., Kalpidis, D. R., Horvath, A., Petrie, A. and Donos, N. (2012) Systematic Assessment of Clinical Outcomes in Bone-Level and Tissue-Level Endosseous Dental Implants. J Oral Maxillofac Implants. 27: 1359-1374. Link: https://pdfs.semanticscholar.org/013a/5b3d054d07a78a5919fdca0df923a79b66af.pdf. [Last accessed: 01.10.18].
[viii]Le, B., Borzabadi-Farahani, A. and Nielsen, B. (2016) Treatments of Labial Soft Tissue Recession Around Dental Implants in the Esthetic Zone Using Guided Bone Regeneration With Mineralised Allograft: A Retrospective Clinical Case Series. Journal of Oral and Maxillofacial Surgery. 74(8): 1552-1561. Link: https://doi.org/10.1016/j.joms.2016.04.015. [Last accessed: 01.10.18].
[ix]Bianchi, A. E., Bosetti, M., Dolci, G. Jr., Sberna, M. T., Sanfilippo, S. and Cannas, M. (2004) In vitro and in vivo follow-up of titanium transmucosal implants with a zirconia collar. J Appl Biomater Biomech. 2(3): 143-150.
No Comments
No comments yet.
Sorry, the comment form is closed at this time.